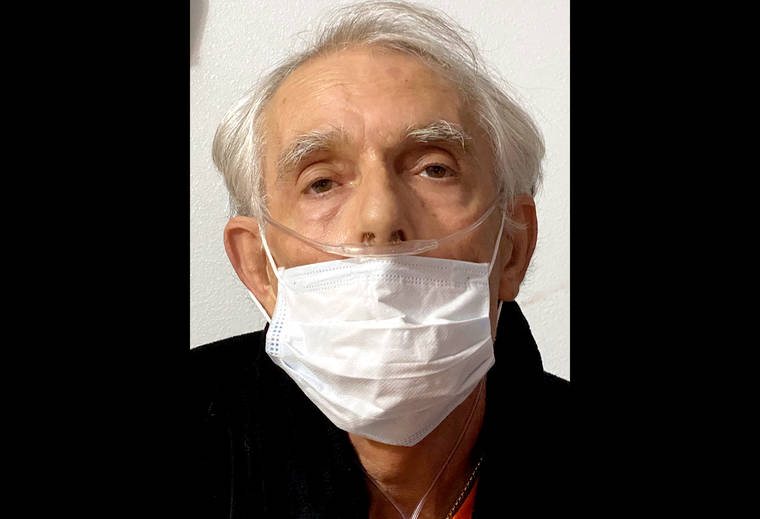
Iam a 68-year old single father from Puna. I have end stage chronic obstructive pulmonary disease, which I’ve been dealing with in some form since 2015. This summer, I was given six months to live.
These days, I often can’t get to the bathroom in time, so I have to keep buckets and towels nearby. This is very disturbing to me. I have a nebulizer to stop my breathing attacks, but they are coming more frequently. Now I use it every two hours. I’m worried one day it just won’t stop them.
I’m coming to the end of my time, but one thing that gives me peace of mind is the fact that I got a prescription for medical aid-in-dying medication. I plan to use it so I can have a peaceful death before my suffering gets to be too much. I’m grateful to the State of Hawaii for passing the Our Care, Our Choice Act (OCOCA) in 2018 which allowed me to do this.
However, I feel I must share my experience trying to find a doctor in East Hawaii to help me use the law, because it was needlessly difficult.
Initially, when I asked my Hilo primary care doctor about using the OCOCA, he told me “I’ll do anything I can to help you.” I was relieved — I had my prescribing doctor (the “attending physician”) lined up. My pulmonologist was understanding and supportive, and while he did not want to be my attending, he did agree to be my “consulting physician,” which is the second doctor the law requires. He told me that if anyone qualified to use the law, it was me.
Under the law, I also had to find a third provider to assess my mental health, which I did. I figured I was ready to go.
When I got my terminal prognosis this summer, I went back to my primary doctor. This time, he declined to be my prescribing doctor. Not only that, but he actually told me if I wanted to die, I could “get a big bottle of Benadryl. That’ll stop your heart.”
I was floored. I felt totally abandoned.
I’m not a computer user, so I spent every day for the next two weeks calling all the doctors in my insurance booklet. I can only talk for a short time in the mornings before my voice gives out, so this was pretty rough. Only two doctors even bothered to call me back, and neither would help. I called our family clinic but the folks there knew nothing about the law and didn’t know where to go for information.
Finally I called people in Oregon, where they have had a law like Our Care Our Choice for about 25 years now. Eventually that led me to Compassion &Choices Hawaii, who helped me find a doctor in North Hawaii who would prescribe the medication.
I had so many hoops to jump through. I had to make two verbal requests for the medicine, 20 days apart, and one in writing. I had to get a mental health assessment. All this time, I was hurting so bad. It took 45 days from my first request to actually having the medication.
What matters to me most in my final days is being able to talk to my daughter, who is a straight-A student and the light of my life, and to her mother, who has come back into my life during this time so she can be there for our daughter’s next phase of her journey without me.
I want to be comfortable, have a little dignity left, and be sane enough to make a little sense. I don’t want my family to see me suffer. I have my “exit date” planned for later this month, and they will be with me when I pass. I appreciate having this small bit of control over my final days.
To our lawmakers and health care providers, I hope that you make it easier for dying people like me to access this compassionate law. It’s cruel to force a suffering, dying person to run around begging doctors to help.
I understand the Department of Health has recommended to the Legislature that qualified nurse practitioners no longer be prohibited from acting as the prescribing provider under the law. I could not agree more, especially for those of us in rural Hawaii who have limited access to MDs.
I won’t be around for the next legislative session, but I hope the law can be fixed so people can actually use it.